Orthopedic surgical blades stand as the unknown heroes of musculoskeletal surgery, enabling surgeons to make precise, controlled cuts in bone, cartilage, and soft tissue. These specialized blades have evolved far beyond basic cutting implements, merging advanced materials science with anatomical expertise to address the unique challenges of orthopedic procedures—from joint replacements to fracture repairs and spinal surgeries. Their ability to balance cutting efficiency with tissue preservation directly impacts surgical success and patient recovery.
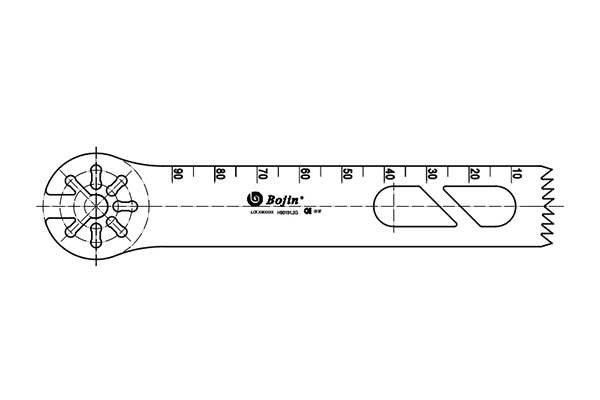
The diversity of orthopedic surgical blades reflects the complexity of the procedures they serve, with three primary types dominating operating rooms. Sagittal saw blades, named for their alignment with the body’s sagittal plane, feature thin, flat profiles and precision-machined serrations. They excel at linear cuts, making them indispensable for shaping femoral and tibial surfaces in knee replacements or preparing bone beds for hip implants. Oscillating blades, by contrast, move in rapid back-and-forth arcs, reducing the risk of tissue tearing—ideal for delicate work like spinal decompression or removing bone spurs near nerves. Specialty blades, such as curved or tapered variants, cater to niche needs, including pediatric orthopedics or maxillofacial bone contouring.
Material innovation is the cornerstone of modern orthopedic blade performance. Most blades are crafted from medical-grade cobalt-chromium alloys or high-strength stainless steel, selected for their exceptional edge retention and resistance to corrosion from bodily fluids. Advanced manufacturing techniques elevate their precision: laser cutting ensures consistent serration geometry, while diamond honing creates ultra-sharp edges that maintain sharpness through prolonged use. Many blades also incorporate titanium nitride coatings, which reduce friction between the blade and bone, minimizing heat generation—a critical feature, as excessive heat can damage bone cells and hinder healing.
Design refinements have further enhanced the utility of these blades. Variable tooth spacing is a key innovation: finer teeth on the blade tip allow for precise entry into delicate tissue, while wider, more aggressive serrations toward the base tackle dense cortical bone efficiently. Ergonomic blade attachments, compatible with powered surgical systems, enable surgeons to adjust cutting speed and pressure—slower speeds for cancellous bone to avoid splintering, faster speeds for cortical bone to boost efficiency. Anti-kickback mechanisms, integrated into many blade designs, prevent sudden movements if the blade encounters unexpected resistance, protecting both patient and surgeon.
Clinical applications of orthopedic surgical blades span the full spectrum of orthopedics. In total knee arthroplasty, sagittal blades shape the femur and tibia with submillimeter accuracy, ensuring prosthetic components fit seamlessly and reduce long-term loosening risks. In trauma surgery, oscillating blades quickly and safely remove damaged bone fragments to stabilize fractures. For spinal fusion procedures, miniaturized specialty blades dissect soft tissue and trim bone without compressing neural structures. Even in sports medicine, these blades facilitate arthroscopic-assisted procedures, minimizing incision size and shortening recovery time.
Quality and safety are non-negotiable standards for these blades. Each unit undergoes rigorous testing, including tensile strength assessments and sterility validation, to meet global medical standards like ISO 13485. Disposable blades eliminate cross-contamination risks, while reusable variants are engineered to withstand multiple high-temperature sterilization cycles without degrading. As AI and robotics integrate into orthopedics, future blades may feature smart sensors to monitor cutting pressure, further elevating precision. In every form, orthopedic surgical blades remain essential tools—bridging engineering innovation and medical expertise to restore mobility and improve lives.